Strabismusis is a very common ocular cause
of visual impairment in optometry and ophthalmology. The prevalence of
strabismus worldwide is reported as 5.7%1. Strabismus or squint is a
disorder in which the eyes are not properly aligned with each other. It involves a lack of coordination
between muscle movements of two eyes. It can be due to either an imbalance of
muscles or disruption in the nerve supply2. Paralytic or incomitant
strabismus occurs when there is limitation of ocular movement. Palsy disrupts
the maintenance of binocular single vision and due to loss of fusional amplitude
resulting in diplopia (double vision) which may be compensated by abnormal head
posture3. Many different treatment options are available to resolve
the issue, including occlusion, refractive correction, prisms, vision therapy
and surgical intervention4.
A paralytic deviation undergoes several
stages. The first stage is characterized by limitation of movement affecting
one muscle, as a rule and secondly by over action of contralateral synergist.
During this stage the law of equal innervation exhibits. The third stage is contracture
of ipsilateral antagonist that shows the reciprocal innervation to the muscle. And
lastly, secondary inhibition of contralateral antagonist occurs because the
contracted antagonist in affected eye requires less innervation. All these
stages result in an angle of deviation which increases on movement of the eyes
in the direction of limitation and decreases when they move away from the affected
side. Moreover secondary deviation is seen which is always greater than primary
deviation. Secondary deviation is assessed by fixing the affected eye while
primary deviation is assessed by fixing the normal eye4.
The paralysis of abducent nerve can be
either congenital or acquired5 and the most common cause of 4th
nerve palsy is congenital6. Common causes for pupil-sparing
pathologies are diabetic neuropathy, myasthenia gravis, atherosclerosis,
chronic progressive ophthalmoplegia and vasculopathies. On the other hand, the
most common causes of non-pupil sparing oculomotor palsy are tumor, followed by
vascular lesions (posterior communicating aneurysms, and then distal basilar
artery aneurysms)7.
The rationale of the
study was to collect data about cases with neurogenic strabismus so that we can
manage them better. This study was carried out to identify patients in the
orthoptic clinic who had ocular motility problems due to
the neurogenic causes.
MATERIAL AND METHODS
It
was hospital-based, cross-sectional study conducted at Orthoptics Clinic of
Al-Ibrahim Eye Hospital (AIEH) Karachi, Pakistan by using non-probability,
convenient sampling technique from May to October 2018. Ethical approval was
given by Research Ethical Committee (REC) of Isra Postgraduate Institute of
Ophthalmology. 349 patients who visited orthoptics clinic
during period of data collection were included. The inclusion criteria were subjects between 5-75 years of age who had manifest neurogenic strabismus, no
history of previous squint surgery or other ocular disease. Subjects with
history of trauma, diabetes and hypertension were included as well. The exclusion criteria
included subjects with latent and puesdo strabismus and syndromes.
All the subjects were
examined after obtaining fully informed written consent. The protocol for
examination for all patients included the demographic data, history of onset,
type of squint. All this was retrieved from the case notes. History revealed
whether the patient had trauma, diabetes or hypertension. Visual acuity of
every patient was checked and recorded separately both for near and distance,
with and without glasses. Then orthoptic assessment was done to evaluate the
type of palsy which included cover/uncover test, ocular motility, prism cover
test and pupillary reflex test. Cover test was assessed to check the eye
affected in primary position, angle and type of tropia with occluder and fixation
targets both in distance and near. Extra-ocular motility test in all gazes was
checked first in versions to check any limitation (underactions) with secondary
angle of deviation (overactions) and then ductions were checked by occluding
one eye to confirm the limitation of gaze. Hess chart was performed to make the
final diagnosis by correlating all the tests results. The anterior segment was
also examined with a slit-lamp by an ophthalmologist to exclude any ocular
disease and the refraction (dry or cycloplegic) was also assessed by optometrist. Data analysis was
done on statistical package for social sciences (SPSS) version 20.0. All
continuous variables were presented as mean ± standard deviation. The entire
categorical variables were shown as frequency and percentages. Statistical
charts were presented in the form of Bar chart & Pie chart.
RESULTS
A total of 21 subjects among 349 subjects fulfilled the inclusion
criteria for the study. Among them, 5 were females, and 16 were males. The mean
age of onset was 35.3 years, ranging between 5-75 years. The frequency of
neurogenic strabismus was found to be 6%. Out of 21 subjects, 8 (38.1%)
subjects were found to have diabetes, 2 (9.5%) subjects had hypertension, 5
(23.8%) subjects had ocular trauma and 6 (28.6%) subjects had other causes as
shown in Figure 1. The most affected eye was right eye in 13 (61.9%) subjects
as shown in Figure 2. At the end of the examination the most commonly seen
manifest deviation on cover test was esotropia in 13 (61.9%) subjects, followed
by exotropia in 4 (19%), hypotropia in 2 (9.5%), hypertropia in 1 (4.8%) and
combined in 1 (4.8%) subject as shown in Figure 3. The diagnosis of all
subjects on Hess chart and other tests showed the most common ocular motor
nerve involved was abducent (sixth) nerve in 13 (61.9%) subjects, followed by
oculomotor (third) nerve in 4 (19%) subjects. Out of the patients who had third
nerve palsy 3 (14.3%) subjects had pupil sparing while only 1 (4.8%) subject had
no pupil sparing. Double elevator palsy was seen in 2 (9.5%) subjects, there
was a single case (4.8%) of fourth nerve palsy and combined nerve involvement
was seen in 1 (4.8%) subject as shown in Figure 4.
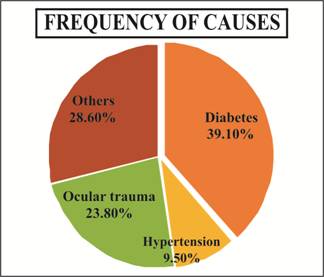
Fig. 1: Frequency of Causes of Palsies.
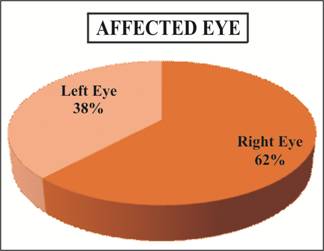
Fig. 2: Distribution
of Affected Eye.
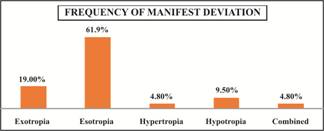
Fig. 3: Frequency of Manifest Type of Deviation on Cover Test.
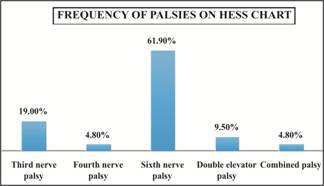
Fig. 4: Frequency of Distribution
of Palsies tested on Hess Chart.